A recent JAMA Network Open study determines whether the coronavirus disease 2019 (COVID-19) pandemic influenced the increase of neonatal mortality in the United States.
Study: Social Distancing During the COVID-19 Pandemic and Neonatal Mortality in the US. Image Credit: Jessica Montgomery / Shutterstock.com
How did the pandemic affect prenatal care?
The COVID-19 pandemic, which was caused by the rapid transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), led to millions of deaths worldwide. To mitigate the effects of the global pandemic, many countries throughout the world implemented regional and national lockdowns, restrictions on public gatherings, stay-at-home restrictions, school and workplace closures, social distancing, mandatory facemasks, and travel restrictions.
Although these strategies reduced the transmission of SARS-CoV-2, they were associated with unanticipated effects, such as reduced healthcare accessibility and utilization, even for people with serious illnesses.
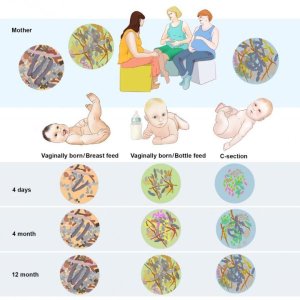
Pregnancy complications increase the risk of neonatal morbidity and preterm delivery. Moreover, pregnant women experienced significant challenges in assessing healthcare facilities during the pandemic. Thus, reduced access to antenatal and perinatal care during the pandemic may have resulted in increased neonatal mortality.
Many studies examining the effects of the COVID-19 pandemic on perinatal, neonatal, and infant outcomes reported inconsistent findings. To date, no studies have evaluated the impact of social distancing during the pandemic on infant outcomes.
About the study
The current population-based cohort study hypothesized that social distancing during the COVID-19 pandemic led to an increase in neonatal mortality rates. Data were obtained from the National Center for Health Statistics (NCHS) of the U.S. Centers for Disease Control and Prevention (CDC) maternal-linked birth and infant death records between January 2016 and December 2020.
The reference period included data obtained between January 2016 and February 2020, whereas the pandemic period comprised data obtained between March 2020 and December 2020. Mortality rates were expressed for every 1,000 live births, and the reference period was estimated as the mean of monthly rates.
Neonatal mortality was defined as death that occurred at less than 28 days of age, whereas early neonatal mortality was defined as death occurring at less than seven days of life. Infant mortality was defined as death at less than 365 days of age.
The gestational age at birth was categorized as extremely preterm at 22-27 weeks, moderately preterm from 28 to 32 weeks, late preterm between 33 and 36 weeks, and term at 37-41 weeks.
An interrupted time-series analysis was performed using machine learning (ML)-based Box and Jenkins autoregressive integrated moving average (ARIMA) models. These models were developed using the reference period data of 50 consecutive months to predict neonatal mortality rates for the pandemic period. The correlation between outcome rates and social distancing index (SDI) was assessed to determine the extent to which an individual adhered to social distancing.
Study findings
No significant association between the SDI and neonatal, early neonatal, infant mortality rates, and births across gestational age categories was identified. This observation was based on 18,011,173 live births, 15,136,596 and 2,874,577 of which occurred during the reference and pandemic periods, respectively.
Infant mortality rates were not significantly associated with the SDI. Notably, a statistically significant correlation between the SDI and higher neonatal and early neonatal mortality with a two-month lag period was observed, along with higher births at 22-27 weeks and 28-32 weeks gestational age with a one-month lag period.
This observation emphasizes the importance of determining the unintended consequences of the COVID-19 pandemic. Clarifying this relationship will help protect the most vulnerable groups, such as pregnant women and infants, from adverse consequences.
Consistent with previous meta-analysis findings, the current study revealed that preterm delivery at less than 37 weeks and neonatal mortality during the pandemic period were not significantly different from the reference period.
Conclusions
The study findings indicate that social distancing implemented during the COVID-19 pandemic did not significantly influence infant health. However, a significant association was observed when considering a two-month lag period. Here, pandemic-period social distancing measures were associated with higher early neonatal mortality and preterm birth rates with a lag period. In the future, more research is needed to understand the interactions of SDI with other pandemic-related indices that may affect infant mortality.
The current study has some limitations, including its observational design that restricted the establishment of causality. Furthermore, there is a possibility of residual unaccounted confounding due to regional variations in pandemic severity and health intervention accessibility. However, the large study cohort and ML-based ARIMA-adjusted analyses increased the reliability of these results.
Journal reference:
- Shukla, V. V., Weaver, L. J., Singh, A., et al. (2024) Social Distancing During the COVID-19 Pandemic and Neonatal Mortality in the US. JAMA Network Open 7(7). doi:10.1001/jamanetworkopen.2024.22995