This kind of market dominance often comes with a plausible sounding–but deeply flawed–rationalization by those who achieve it. As an example, here is a video of the president of Massachusetts General Hospital describing why their high rates were necessary and how they used the creation of Partners to achieve this result.
Start at minute 42:00 when the question is asked and follow through for just five minutes. Listen carefully to the response. As you face similar issues in your region of the country, it’s important to deconstruct what’s being said and what isn’t being said.
I’ll paraphrase portions of the answer, add emphasis, and reorder things to create some adjacencies for purposes of this discussion:
One of the reasons that Partners was created was that the insurance companies were playing MGH and the Brigham off against each other. We came together and now insurers have to take both of us or neither of us and that has helped level the playing field with the insurers.
We built an organization that could level the playing field with the insurers. Unfortunately, not many other provider organizations in this state did that, and now we’re viewed as the problem when we negotiated rates that we thought were reasonable and others didn’t become more indispensable and didn’t increase their leverage vis-a-vis the payers and weren’t able to get rates as high as ours.
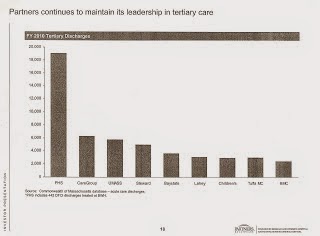
This is what market dominance looks like, a chart showing the size of PHS relative to other healthcare systems in the state:
The creation of Partners was not just about joining the two tertiary hospitals into one group. The merger also brought in a number of community doctors and thousands of physicians. Those tertiary discharges shown above are the result of this immense referral network. While it might have been theoretically possible to create another system of comparable size, it was not practical to do so.
Indeed, once PHS had higher rates, it could pay more to unaffiliated community-based doctors and grow its referral base even further, building still more market power.
What were those rate “requests?”
We were very judicious in what we asked for. We compared our rates with other teaching hospitals around the country that we compete with–Johns Hopkins, Mayo, Cleveland Clinic, etc.–and we set out to get reimbursement that covered [our] costs
Similarly on physician contracts. We did some studying to see what academic physicians in other parts of the country were getting. We were losing physicians because we couldn’t match salaries in Cleveland etc. So we set out to get physician salaries that were comparable to other parts of the country.
Putting aside whether there is really much competition for patients across the country, seeking rates based on other regions in which other dominant systems exist was merely using other monopoly pricing power to justify the results that Partners sought here. In addition, PHS was not just setting rates for its academic functions. Those high paying insurance contracts also covered the PHS community hospitals and community-based doctors. The leverage gained was system wide, not just for the two tertiary centers.
When Blue Cross Blue Shield balked during the first PHS negotiation at the level of rates, PHS CEO Sam Thier’s words to the CEO of BCBS were, “This is what good health care costs.” The insurance company acceded. When Tufts Health Plan balked, PHS simply threatened to leave them out of the network. Tufts folded with 72 hours.
Recall this comment from 2010 to understand the persistence of the degree of market power exercised:
“Andrew Dreyfus, executive vice president of health care service for Blue Cross Blue Shield of Massachusetts – the state’s largest insurer – said he doesn’t believe his company has the market power to eliminate disparities in the way doctors and hospitals are paid for their services.”
If you look at markets around the country, in every market there is variability in payments. For example, in New Hampshire, Dartmouth has very high rates. Premiums in MA are fourth highest in NE, not highest.
Yes, there is variability. But it is in the range of five, or maybe 10 percent. In Massachusetts, PHS’ rates can be 30{c754d8f4a6af077a182a96e5a5e47e38ce50ff83c235579d09299c097124e52d} or more above those paid to other hospitals and doctors.
And note how he then he switches from rates to premiums. Premiums are based on the total mix of payments made by insurers, across all providers. A focus on premiums masks the fact that because PHS rates are higher, those to other hospitals and doctors are forced down.
And then the ultimate canard:
What we’ve done with those rates. Our psychiatry program is one example. If our rates get cut dramatically, that’s in jeopardy. Ditto for five neighborhood health centers caring for the poor. We have to invest in infrastructure to support our research program, the largest in the country. We use our rates to help support our research program. We invest in a lot of public goods as result of those rates.
Teaching hospitals have special mission: research, education, specialized units, taking care of more poor people. That’s what’s in jeopardy if our rates are equalized with community hospitals.
Notice how the conversation is switched to one of apples and oranges–what MGH should be paid relative to other system’s community hospitals. The reports produced by the Attorney General did not suggest that the rates for PHS academic centers were too high relative to community hospitals: The showed that they were too high relative to the other academic centers–all of whom offer the public goods as well. The analyses also showed that the rates paid to the PHS community hospitals were too high relative to other community hospitals. They also showed that rates paid to PHS community doctors were too high relative to those paid to other community doctors.
The evidence from Massachusetts is that once you let the market power horse out, it will be too late to close the barn door. Notwithstanding consistent evidence of the adverse impact on healthcare costs from PHS’ dominance, there is no state action that has reversed it. Indeed, recent “cost control” legislation in the state is a nullity when it comes to reducing the disparity in provider rates in the state. By its language, the law bakes in the PHS advantage. By its interpretation thus far, it has done even worse, permitting PHS to have a larger increase on a larger base than other systems.
Here’s hoping it is not too late in your state.
SOURCE: Not Running a Hospital – Read entire story here.